
3. The Significance of Repeated Education in Correcting Insulin Injection Techniques and Improving Glycemic Control |

![]() This original research was presented by Dr.Jothydev Kesavadev at San Diego, USA at the 77th Scientific Sessions of American Diabetes Association in June 2017 from Jothydev’s Diabetes & Research Centres, Kerala.
This original research was presented by Dr.Jothydev Kesavadev at San Diego, USA at the 77th Scientific Sessions of American Diabetes Association in June 2017 from Jothydev’s Diabetes & Research Centres, Kerala.
![]() Background: Every patient with diabetes whatever be the type, might require insulin therapy for their disease management. The success of insulin therapy in achieving glycemic control highly relies on proper insulin injection practices. Incorrect injection sites and improper injection techniques will alter insulin absorption thereby leading to treatment flaws such as maximum glucose load and peak insulin effect thus increasing the chances of unexpected hyperglycemia and an increased risk of nocturnal hypoglycemia. Our diabetes center is backed with a qualified and dedicated health management team which consists of clinicians, diabetes educators, dieticians, nurses, pharmacists and device technicians. During each of the in-clinic visits, as well through e-mail or telephonic follow-ups by means of our Diabetes Tele-Management System (DTMS®), all the patients are routinely taught on proper injection practices by our certified diabetes educators. However, even after continuous diabetes education and training, certain patients commit errors in at least some of these techniques.
Background: Every patient with diabetes whatever be the type, might require insulin therapy for their disease management. The success of insulin therapy in achieving glycemic control highly relies on proper insulin injection practices. Incorrect injection sites and improper injection techniques will alter insulin absorption thereby leading to treatment flaws such as maximum glucose load and peak insulin effect thus increasing the chances of unexpected hyperglycemia and an increased risk of nocturnal hypoglycemia. Our diabetes center is backed with a qualified and dedicated health management team which consists of clinicians, diabetes educators, dieticians, nurses, pharmacists and device technicians. During each of the in-clinic visits, as well through e-mail or telephonic follow-ups by means of our Diabetes Tele-Management System (DTMS®), all the patients are routinely taught on proper injection practices by our certified diabetes educators. However, even after continuous diabetes education and training, certain patients commit errors in at least some of these techniques.
![]() Aims: We did a retrospective analysis to understand the impact of brief education sessions in inculcating proper insulin injection practices among our T2DM patients. Beneficial effects of such a session in bringing down improper injection practices and improving diabetes treatment outcomes were assessed.
Aims: We did a retrospective analysis to understand the impact of brief education sessions in inculcating proper insulin injection practices among our T2DM patients. Beneficial effects of such a session in bringing down improper injection practices and improving diabetes treatment outcomes were assessed.
![]() Methods: From our T2DM patients, we identified those individuals who visited the clinic during September 2015 to January 2016 and exhibited faults in their insulin injecting techniques despite attending the routine 15-minute education sessions during their previous visits. Patients were asked to fill in a questionnaire as well as their injection sites were examined. They were again made to attend the session and followed up for the succeeding 6 months to understand the underlying benefits of such training episodes. Patients continued to receive treatment, lifestyle, and disease management advice frequently by means of the unique DTMS® as a part of our routine clinical practice. Clinical profile of these patients at baseline and at their 6th month visit was procured from electronic medical records.
Methods: From our T2DM patients, we identified those individuals who visited the clinic during September 2015 to January 2016 and exhibited faults in their insulin injecting techniques despite attending the routine 15-minute education sessions during their previous visits. Patients were asked to fill in a questionnaire as well as their injection sites were examined. They were again made to attend the session and followed up for the succeeding 6 months to understand the underlying benefits of such training episodes. Patients continued to receive treatment, lifestyle, and disease management advice frequently by means of the unique DTMS® as a part of our routine clinical practice. Clinical profile of these patients at baseline and at their 6th month visit was procured from electronic medical records.
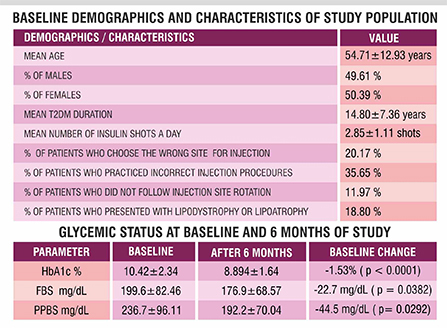
![]() Results: Among T2DM patients, 126 individuals were identified with wrong injection practices. Patient demographics at the start of the study were- Mean age 54.71±12.93 years, Males 49.61 %, T2DM duration 14.80±7.36 years, mean HbA1c 10.42±2.33%, mean FBS 199.60±82.46 mg/dL, mean PPBS 236.70±96.11 mg/dL, average number of insulin shots a day 2.85±1.11. The site of injection was incorrect in 20.17% of the patients, in 35.65% procedure of injecting was incorrect and 11.97% did not follow injection site rotation. 18.80 % of the patients presented with lipodystrophy or lipoatrophy. A significant correlation was noted between the presence of lipodystrophy or lipoatrophy and different factors such as the site of injection (p = 0.0071), injection site rotation (p = 0.0007), and proper injecting procedure (p = 0.0044). After 6 months, significant mean changes from baseline were observed among these patients for HbA1c (-1.53%), FBS (-22.7 mg/dL) and PPBS (-44.5 mg/dL).
Results: Among T2DM patients, 126 individuals were identified with wrong injection practices. Patient demographics at the start of the study were- Mean age 54.71±12.93 years, Males 49.61 %, T2DM duration 14.80±7.36 years, mean HbA1c 10.42±2.33%, mean FBS 199.60±82.46 mg/dL, mean PPBS 236.70±96.11 mg/dL, average number of insulin shots a day 2.85±1.11. The site of injection was incorrect in 20.17% of the patients, in 35.65% procedure of injecting was incorrect and 11.97% did not follow injection site rotation. 18.80 % of the patients presented with lipodystrophy or lipoatrophy. A significant correlation was noted between the presence of lipodystrophy or lipoatrophy and different factors such as the site of injection (p = 0.0071), injection site rotation (p = 0.0007), and proper injecting procedure (p = 0.0044). After 6 months, significant mean changes from baseline were observed among these patients for HbA1c (-1.53%), FBS (-22.7 mg/dL) and PPBS (-44.5 mg/dL).
For enquiries info@jothydev.net.
Please visit: jothydev.net | research.jothydev.com | diabscreenkerala.net | jothydev.com/newsletter
