2. Pancreatic stem cell therapy – A revolutionary approach to diabetes cure
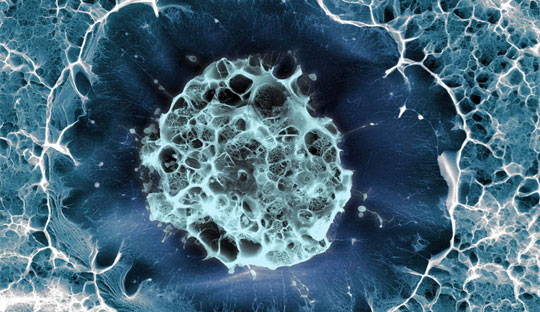
Ever since its discovery, insulin remains as the mainstream therapy for diabetes. However, with the advances in diabetes technologies and therapeutics, the scenario is slightly shifting towards employing innovative approaches for diabetes management. A recent study that explored the potential of pancreatic progenitor (PP) cells or islet tissues, generated from human pluripotent stem cells (hPSCs) in animal models shows exiting results in reducing hyperglycaemia. Progressive research with these findings resulted in testing the impact of islet tissues in people with diabetes and identifying intermediate stem cell types, including the non-tumorigenic human endoderm stem cells (EnSCs), which appear to be more suitable as precursors for large-scale generation of islet cells.
The pilot study published in ‘Cell Discovery’, investigated the safety and efficacy of E-islets for the treatment of insulin-dependent 59 year old patient with t a 25 years history of type 2 diabetes. The patient developed end-stage diabetic nephropathy and underwent kidney transplantation and expressed poor glycemic, characterized by blood glucose level ranging from 65.95–263.06 mg/dL, mean amplitude of glycemic excursion (MAGE) of 99.82 mg/dL, the time-in-the-tight-target-range (TITR, 3.9–7.8 mM) of 56.7%, with daily hyperglycemic events (> 180.18 mg/dL) of 0.7/d and hypoglycemic events (< 70.27 mg/dL) of 0.3/d. Due to the major concerns of hypoglycemia and the detrimental effect of poor glycemic control on the long-term survival of the donor kidney, the patient agreed to pursue transplantation with autologous E-islets.
E-islets were generated from the autologous EnSCs that are established under the culture condition. The patient-specific E-islets survived and functioned under the kidney capsules of the diabetic immunocompromised mice humanized with patient’s own PBMCs, but rejected by the ones humanized with PBMCs from an unrelated volunteer which suggests that patient’s immune system likely tolerates the autologous E-islets. The patient underwent a percutaneous transhepatic portal vein transplantation with 1.2 million IEQs of E-islets delivered, conforming to the regulatory guidance from the clinical islet transplantation registration. During the pre-set follow-up visits, examinations of endocrine function and diabetes-specific parameters by mixed-meal tolerance test (MMTT) were performed at baseline, 4, 8, 12, 16, 20, 24, 36 and 48 weeks and thereafter at specified time. The glycemic control of the patient was measured with a 24-h real-time continuous glucose monitoring system (CGM).
The three major clinical outcomes, the glycemic targets, the reduction of exogenous insulin and the levels of fasting and meal-stimulated circulating C-peptide/insulin were monitored throughout the first 116 weeks. Remarkable changes in the patient’s glycemic control were observed as early as week 2 post transplantation, as the MAGE declined from 99.09 mg/dL to 64.86 mg/dL, and the TITR increased rapidly from 56.7% to 77.8%. Over the same period, the time-above-range (TAR) decreased by 55% from baseline, while the events of severe hyperglycemia (> 13.9 mM) and hypoglycemia (< 3.9 mM) completely disappeared. During the period between weeks 4 and 12, a significant reduction in ambulatory mean glucose fluctuations (from 99.1 to 46.85 mg/dL) and a steady rise in TITR (from 81% to 90%) were observed. After week 32, the patient’s TITR had readily reached 99% and was maintained thereafter), while MAGE, reduced from 5.50 mM to 1.60 mM. Most importantly, no episodes of hypoglycemia or severe hyperglycemia were observed during the whole follow-up period of 116 weeks post surgery The MMTT revealed a trend of stabilization in glycemic variability after surgery, as manifested by the stable fasting glucose concentrations and the significant reductions in the post-meal glucose concentrations Notably, the insulin requirements were reduced gradually until complete withdrawal at the end of week, and the oral antidiabetic medications were tapered since week 44 and discontinued at weeks 48 (acarbose) and 56 (metformin).
In summary, the study is the first-in-human tissue replacement therapy using autologous E-islets for a T2D patient with impaired islet function.
For enquiries info@jothydev.net.
Please visit: jothydev.net | research.jothydev.com | diabscreenkerala.net | jothydev.com/newsletter