3. Remission of T2DM after Bariatric Surgery is characterized |
![]() Adults who underwent bariatric surgery and were in type 2 diabetes remission demonstrated high glycemic variability and oxidative stress, according to findings published in Nutrition, Metabolism & Cardiovascular Diseases.
Adults who underwent bariatric surgery and were in type 2 diabetes remission demonstrated high glycemic variability and oxidative stress, according to findings published in Nutrition, Metabolism & Cardiovascular Diseases.
![]() Brunella Capaldo, MD, of the department of clinical medicine and surgery at Federico II University in Naples, Italy, and colleagues evaluated 22 adults (10 men; mean age, 50 years; mean BMI, 31 kg/m2) who were in remission of type 2 diabetes after bariatric surgery and 22 age-, sex- and BMI-matched controls to assess glycemic variability and oxidative stress. Mean postoperative follow-up was 4 years. Among the bariatric surgery group, 11 underwent Roux-en-Y gastric bypass (RYGB) and 11 underwent sleeve gastrectomy.
Brunella Capaldo, MD, of the department of clinical medicine and surgery at Federico II University in Naples, Italy, and colleagues evaluated 22 adults (10 men; mean age, 50 years; mean BMI, 31 kg/m2) who were in remission of type 2 diabetes after bariatric surgery and 22 age-, sex- and BMI-matched controls to assess glycemic variability and oxidative stress. Mean postoperative follow-up was 4 years. Among the bariatric surgery group, 11 underwent Roux-en-Y gastric bypass (RYGB) and 11 underwent sleeve gastrectomy.
![]() Researchers evaluated oral glucose tolerance testing, 7 days of continuous glucose monitoring, 24-hour urinary excretion of 8-iso-prostaglandin F2 alpha and dietary intake.
Researchers evaluated oral glucose tolerance testing, 7 days of continuous glucose monitoring, 24-hour urinary excretion of 8-iso-prostaglandin F2 alpha and dietary intake.
![]() During OGTT, glucose response was higher in the remission group compared with controls (P < .001), and the difference in plasma glucose level was evident at 30 and 60 minutes of the test (P = .01 for both). A difference was observed between the two groups for insulin response (P < .001). Compared with the control group, plasma insulin level at 120 minutes was lower in the remission group (P < .05).
During OGTT, glucose response was higher in the remission group compared with controls (P < .001), and the difference in plasma glucose level was evident at 30 and 60 minutes of the test (P = .01 for both). A difference was observed between the two groups for insulin response (P < .001). Compared with the control group, plasma insulin level at 120 minutes was lower in the remission group (P < .05).
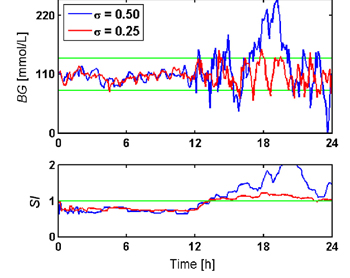
![]() Throughout the CGM period, mean interstitial glucose concentration was similar between the two groups, but mean interstitial glucose peak was higher in the remission group compared with the control group (P< .05). Participants in the remission group who underwent RYGB had lower mean interstitial glucose nadir compared with controls (P < .05). The remission group had higher measures assessing the amplitude of glycemic variability, including standard deviation of blood glucose, coefficient of variation and mean amplitude of glucose excursions vs. the control group (P < .05 for all). Compared with participants in remission who underwent sleeve gastrectomy, participants in remission who underwent RYGB had greater glycemic variability (coefficient of variation, P < .05; mean amplitude of glucose excursions, P < .05).
Throughout the CGM period, mean interstitial glucose concentration was similar between the two groups, but mean interstitial glucose peak was higher in the remission group compared with the control group (P< .05). Participants in the remission group who underwent RYGB had lower mean interstitial glucose nadir compared with controls (P < .05). The remission group had higher measures assessing the amplitude of glycemic variability, including standard deviation of blood glucose, coefficient of variation and mean amplitude of glucose excursions vs. the control group (P < .05 for all). Compared with participants in remission who underwent sleeve gastrectomy, participants in remission who underwent RYGB had greater glycemic variability (coefficient of variation, P < .05; mean amplitude of glucose excursions, P < .05).
![]() The remission group had higher mean 24-hour urinary 8-iso-prostaglandin F2 alpha compared with the control group (P = .04). Both groups had similar intakes of total carbohydrates, fat and protein and similar dietary glycemic index and glycemic load.
The remission group had higher mean 24-hour urinary 8-iso-prostaglandin F2 alpha compared with the control group (P = .04). Both groups had similar intakes of total carbohydrates, fat and protein and similar dietary glycemic index and glycemic load.
For enquiries info@jothydev.net.
Please visit: jothydev.net | research.jothydev.com | diabscreenkerala.net | jothydev.com/newsletter
